How I Stopped Getting Sick Every Season – My Real Immunity Journey
Remember that friend who never catches a cold, even in flu season? I used to envy them—until I stopped being the person always bundled up, sneezing through winter. After years of constant sniffles and low energy, I dug into how to truly support my immune system. This isn’t about miracle fixes. It’s what actually worked: small, science-backed changes in sleep, food, and daily habits. If you’re tired of feeling run down, this guide shares the real shifts that helped me build lasting resilience—naturally and consistently.
The Wake-Up Call: When "Always Tired" Became a Problem
For years, I accepted being the first to catch every cold as just part of who I was. It started in my early thirties—back-to-back respiratory infections, lingering fatigue that lasted weeks, and a growing dependence on over-the-counter remedies just to function. My routine included frequent doctor visits, where blood tests showed nothing alarming, yet I felt far from healthy. I dismissed it as stress or aging, but deep down, I knew something was off. The turning point came during a family trip when I spent most of it in bed, missing moments I couldn’t get back. That’s when I realized: being frequently unwell wasn’t normal—it was a signal.
What I didn’t understand then was that immunity isn’t just about avoiding illness; it’s about how well your body responds to daily challenges. Chronic low-grade inflammation, poor recovery, and persistent fatigue are signs of a strained immune system, even without a diagnosed condition. Research shows that repeated infections can weaken the body’s ability to respond effectively over time, making each episode harder to shake. I began to see that my lifestyle—irregular sleep, processed meals, and high stress—wasn’t just affecting my mood; it was directly undermining my body’s defenses.
Many women in their thirties and beyond face similar patterns. Juggling family, work, and personal responsibilities often means self-care comes last. But the truth is, your immune system doesn’t operate in isolation. It’s deeply influenced by how you live each day. The idea that some people are just “lucky” to stay healthy is misleading. Science increasingly shows that immune resilience is shaped by consistent habits, not genetics alone. My journey began not with a dramatic overhaul, but with a simple decision: to stop accepting constant illness as inevitable.
Immunity Demystified: What It Really Means (And What It Doesn’t)
When we talk about immunity, many imagine a shield that either works or doesn’t. But the immune system is not a single force; it’s a complex network of cells, tissues, and signaling molecules working in coordination. It has two main branches: the innate immune system, which acts as the first responder to threats like viruses and bacteria, and the adaptive immune system, which learns from past exposures and creates long-term protection. Together, they patrol the body, identify invaders, and mount responses—all while distinguishing between harmful pathogens and the body’s own healthy cells.
A key misconception is that stronger immunity means a hyperactive system. In reality, an overactive immune response can be just as problematic as a weak one, leading to allergies, inflammation, or autoimmune conditions. True immune health is about balance—keeping the system alert and ready without pushing it into overdrive. Think of it like a well-trained security team: they don’t need to panic at every sound, but they must respond quickly and appropriately when a real threat appears.
White blood cells, including neutrophils, macrophages, and lymphocytes, are central players in this process. They circulate through the bloodstream and lymphatic system, constantly surveying for danger. When they detect a pathogen, they release signaling proteins called cytokines that coordinate the response. Immune memory—how the body “remembers” past infections—is what makes vaccines effective and why you rarely get the same illness twice. But this system doesn’t work well if it’s chronically fatigued by poor sleep, poor nutrition, or ongoing stress.
Understanding immunity as a dynamic, responsive system changes how we approach it. It’s not about “boosting” it with quick fixes, but about creating the conditions for it to function optimally. This means supporting it through lifestyle choices that enhance its efficiency, accuracy, and recovery. The goal isn’t to eliminate all germs—exposure is natural and necessary—but to ensure your body can handle them without collapsing into prolonged illness.
The Sleep-Immunity Link: Why Rest Is Your First Defense
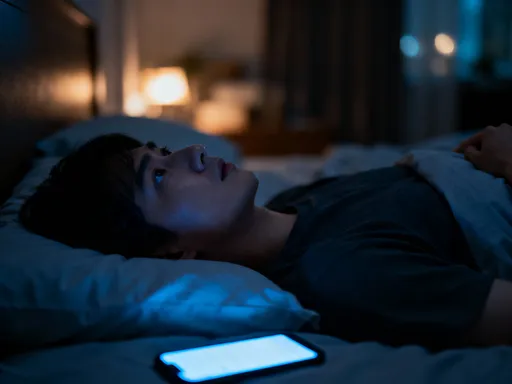
One of the most powerful, yet often overlooked, pillars of immune health is sleep. During deep sleep, the body produces and releases cytokines, proteins that help regulate immune responses. Some of these cytokines are specifically targeted at fighting infection and inflammation. When you’re sleep-deprived, your body produces fewer of these protective molecules, making you more vulnerable to illness. Studies have shown that people who consistently sleep less than six hours per night are more likely to catch colds than those who get seven or more hours.
Sleep also supports the function of T-cells, a type of white blood cell critical for identifying and destroying infected cells. Research has found that T-cell activity is enhanced during rest, particularly during slow-wave sleep. When sleep is disrupted, this process slows down, weakening the body’s ability to respond quickly to threats. Even a single night of poor sleep can impair immune function, which is why many people get sick after periods of stress or travel, when sleep routines are thrown off.
Creating a sustainable sleep routine doesn’t require perfection, but consistency. I started by setting a fixed bedtime and wake-up time, even on weekends, to regulate my body’s internal clock. I also reduced screen exposure at least an hour before bed, since blue light from phones and tablets suppresses melatonin, the hormone that signals sleep. Instead, I began reading or practicing gentle stretching, which helped signal to my body that it was time to wind down.
My bedroom environment also needed attention. I invested in blackout curtains, kept the room cool, and minimized noise. These small changes made a noticeable difference in how quickly I fell asleep and how rested I felt in the morning. Over time, I observed fewer midday crashes and a stronger ability to recover from minor exposures—like being near someone who was sick—without getting ill myself. Sleep isn’t a luxury; it’s a foundational layer of immune defense, and improving it was one of the most effective steps I took.
Food as Fuel: Eating for Immune Resilience, Not Perfection
Nutrition plays a central role in how well the immune system functions. The body relies on a steady supply of vitamins, minerals, and antioxidants to produce immune cells and regulate their activity. Key nutrients like vitamin C, vitamin D, zinc, and selenium are involved in everything from antibody production to inflammation control. Rather than chasing trendy “superfoods” or extreme diets, I focused on building a balanced, whole-foods-based eating pattern that supported long-term resilience.
Vitamin C, found in citrus fruits, bell peppers, and broccoli, supports the skin’s barrier function and enhances the movement of white blood cells. While it won’t prevent a cold, consistent intake helps the body respond more effectively when challenged. Vitamin D, primarily synthesized through sun exposure but also found in fatty fish and fortified foods, is crucial for immune regulation. Low levels have been linked to increased susceptibility to infections, particularly respiratory ones. Zinc, present in legumes, nuts, and whole grains, aids in the development and function of immune cells, especially during the early stages of infection.
But beyond individual nutrients, I learned that gut health is deeply intertwined with immunity. About 70% of the immune system resides in the gut-associated lymphoid tissue, making the digestive tract a major site of immune activity. A diverse gut microbiome—supported by fiber-rich foods like vegetables, fruits, and whole grains—helps maintain a balanced immune response. Fermented foods such as yogurt, kefir, sauerkraut, and kimchi introduce beneficial bacteria that support this ecosystem. I began incorporating a serving of fermented food daily and increased my fiber intake gradually to avoid discomfort.
I also reduced processed foods, added sugars, and excessive saturated fats, which can promote inflammation and disrupt immune balance. Instead of strict rules, I adopted a flexible approach: most meals centered around vegetables, lean proteins, and healthy fats, with room for occasional treats. This wasn’t about achieving dietary perfection, but about creating a pattern that nourished my body consistently. Over months, I noticed fewer digestive issues, more stable energy, and a reduced frequency of colds—proof that food truly is medicine when used wisely.
Movement That Matters: How Daily Activity Supports Your Immune System
Physical activity is another cornerstone of immune health, but not all exercise is created equal. Moderate, regular movement enhances circulation, allowing immune cells to travel more efficiently throughout the body. This improved surveillance means threats can be detected and addressed faster. Studies have shown that people who engage in regular moderate exercise—such as brisk walking, cycling, or swimming—experience fewer upper respiratory infections than sedentary individuals.
I started with simple daily walks, aiming for 30 minutes most days of the week. At first, it felt like just another task, but over time, it became a cherished part of my routine. Walking outdoors added the benefit of fresh air and natural light, both of which support circadian rhythm and mood. I also incorporated light strength training twice a week, using bodyweight exercises like squats, lunges, and push-ups. These helped build muscle, which in turn supports metabolic health and immune function.
Stretching and gentle yoga became part of my evening routine, helping me unwind and improve flexibility. These low-impact activities may not feel intense, but they contribute to overall well-being by reducing physical tension and supporting joint health. The key was consistency, not intensity. I avoided pushing myself to exhaustion, knowing that prolonged, high-intensity workouts without adequate recovery can actually suppress immune function by increasing stress hormones like cortisol.
Finding joy in movement made all the difference. Instead of viewing exercise as punishment or a chore, I reframed it as an act of care. Dancing while cooking, taking the stairs, or playing with my kids in the yard—all counted. The goal wasn’t to train for a marathon, but to keep my body active and resilient. Over time, I noticed improved stamina, better sleep, and a stronger sense of physical confidence. Movement, when done mindfully and regularly, became one of the most reliable tools in my immune-support toolkit.
Stress, Mindset, and the Hidden Immune Cost
Perhaps the most surprising discovery in my journey was how deeply stress affects immunity. Chronic stress—whether from work, family demands, or unresolved worries—triggers a continuous release of cortisol, the body’s primary stress hormone. In short bursts, cortisol helps manage challenges by suppressing non-essential functions, including parts of the immune response. But when stress is constant, this suppression becomes prolonged, weakening the body’s ability to fight off infections.
Research has shown that people under chronic stress are more likely to get sick and take longer to recover. Stress can also disrupt sleep, alter gut bacteria, and lead to unhealthy coping behaviors like poor eating or inactivity—all of which further strain the immune system. I realized that my constant “on-the-go” mentality, while admirable in some ways, was silently undermining my health. I needed to address not just my body, but my mind.
I began with small mindfulness practices. Each morning, I spent five minutes focusing on my breath, observing thoughts without judgment. This simple act helped me start the day with greater clarity and calm. I also used breathing exercises during stressful moments—inhaling slowly for four counts, holding for four, exhaling for six. This technique activates the parasympathetic nervous system, signaling the body to relax.
Spending time in nature became another powerful tool. Even a short walk in a park or sitting under a tree helped reset my mood and reduce mental clutter. I prioritized activities that brought me joy: reading, gardening, or simply sitting with a cup of tea in silence. These moments weren’t luxuries; they were necessary for restoring balance. Over time, I became more aware of my stress triggers and learned to respond with intention rather than reaction. As my mental well-being improved, so did my physical health—fewer colds, more energy, and a greater sense of stability.
Building Your Routine: Small Steps, Big Long-Term Shifts
Integrating all these changes didn’t happen overnight. I started by focusing on one area at a time—first sleep, then nutrition, then movement. I tracked small improvements: fewer nighttime awakenings, more energy in the afternoon, quicker recovery after a busy day. These subtle shifts built confidence and motivation to keep going. I learned that lasting change comes not from drastic overhauls, but from consistent, manageable choices repeated over time.
I created a simple daily rhythm that included fixed sleep times, meal planning, short walks, and mindful moments. I allowed flexibility—life happens, and perfection wasn’t the goal. What mattered was returning to my habits after disruptions. I also learned to listen to my body, recognizing when I needed rest or nourishment. This self-awareness became a form of empowerment, helping me make choices that supported my long-term well-being.
Support played a role too. I shared my goals with my family, who began joining me in walks or trying new recipes. Having allies made the journey less lonely and more enjoyable. I also consulted my healthcare provider before making significant changes, especially regarding vitamin D levels and overall health screening. Professional guidance ensured I was making safe, informed decisions.
Looking back, the most important lesson was patience. Immune resilience isn’t built in a week or a month. It’s the result of daily habits compounding over time. I no longer fear flu season. I’m not perfect—I still get tired, still face stress—but I recover faster and stay healthier overall. The changes I made weren’t about chasing an ideal, but about honoring my body’s needs and creating a life where health could thrive.